Research Phase
PROJECT BRIEF
At first glance, our brief focused on a seemingly simple central question: how might we improve EMR mastery among Sunrise’s users?
Dissecting the brief as a group, we quickly realized how critical it would be for us to develop domain knowledge. As we conducted preliminary research, we faced a veritable alphabet soup of acronyms (e.g. MU, FHIR, HL-7, ICD-10… the list goes on) which we barely understood.

We started drafting a research plan. To cover ground quickly, we assigned owners among ourselves. To make sure that we shared insights, we scheduled interactive lightning talks into our team meetings, where the presenter would summarize findings and the rest of the group would ask questions.
There were also a number of questions and unknowns regarding the brief, which we wouldn’t be able to really answer until we met our clients. How much did our client expect us to focus narrowly on goals like identifying “a systematic approach to deliver in situ learning” versus something broader, like tackling the root causes of usability issues facing EHR systems?
Client Kickoff
When the day finally came, we were greeted with a pleasant surprise: Lisa Khorey, the project’s executive sponsor, would attend after all. She enthusiastically endorsed the project and set a broad scope for the project, challenging us to think both strategically and creatively.

Our takeaway was that, although the overarching goal was clear (i.e. improve EHR mastery and satisfaction among Sunrise’s users), we had an opportunity to formulate our own understanding of the problem, hopefully in a way that pushed our client’s own thinking. Secondly, this project wasn’t just a “blue sky” conceptual project. They wanted a solution which could be feasibly implemented and deliver value after our engagement.
We left the meeting feeling empowered and excited to tackle the challenge ahead.
Research Plan
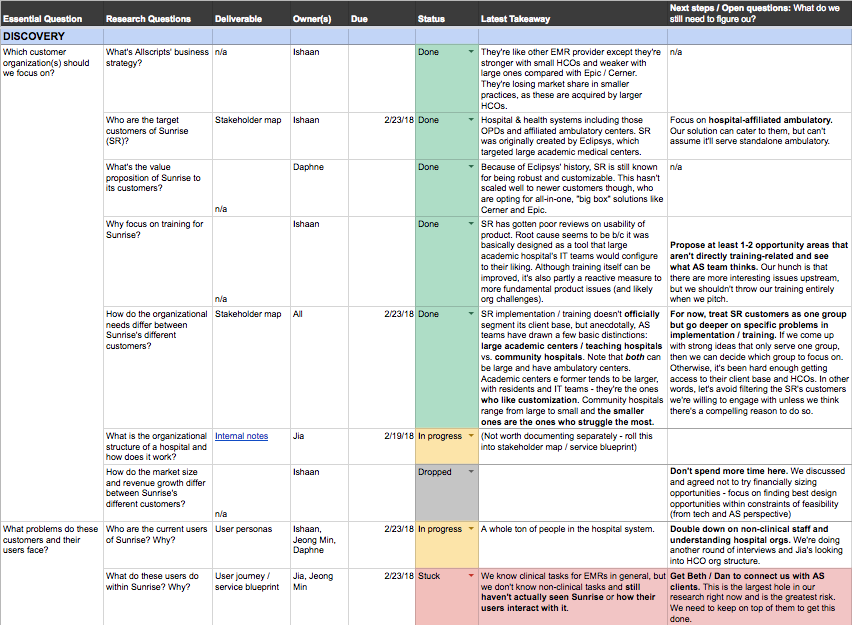
Our research plan was organized into a set of high-level questions and hunt statements, with more specific sub-questions beneath them.
We identified methods which would be best-suited for certain types of questions. For example, we thought that a combination of semi-structured interviews (which could be done remotely) and contextual inquiry within a healthcare setting would help us explore the roles, activities, and environmental context of EHR workflows.
A critical piece of advice that we received early on from a business executive in the health IT space was to be very specific about the type of healthcare setting and roles that we would focus on. The number of users, healthcare organizations, vendor relationships, and implementation scenarios in the EHR space can be overwhelming. Without a clear focus, there’s a real risk of developing a “mile wide, inch deep” understanding of the problem space.
We kept this advice in mind as we pushed forward into our discovery phase. As we scheduled exploratory interviews, we made it a point to gather as much data as possible about the interviewees organizational context, in addition to their personal experience. This enabled us to gradually develop a more nuanced understanding of the people and usage scenarios surrounding EMRs across multiple healthcare settings.
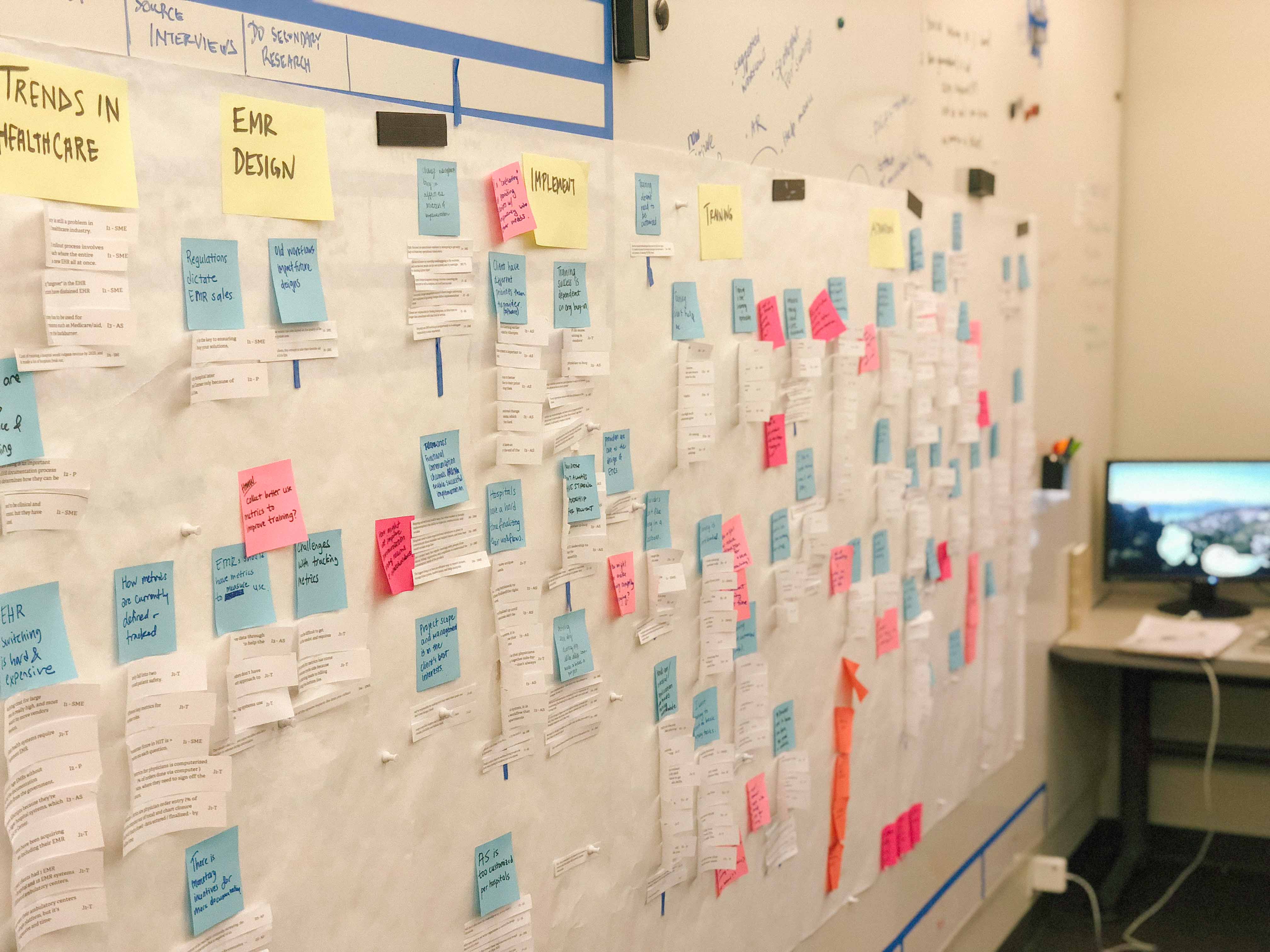
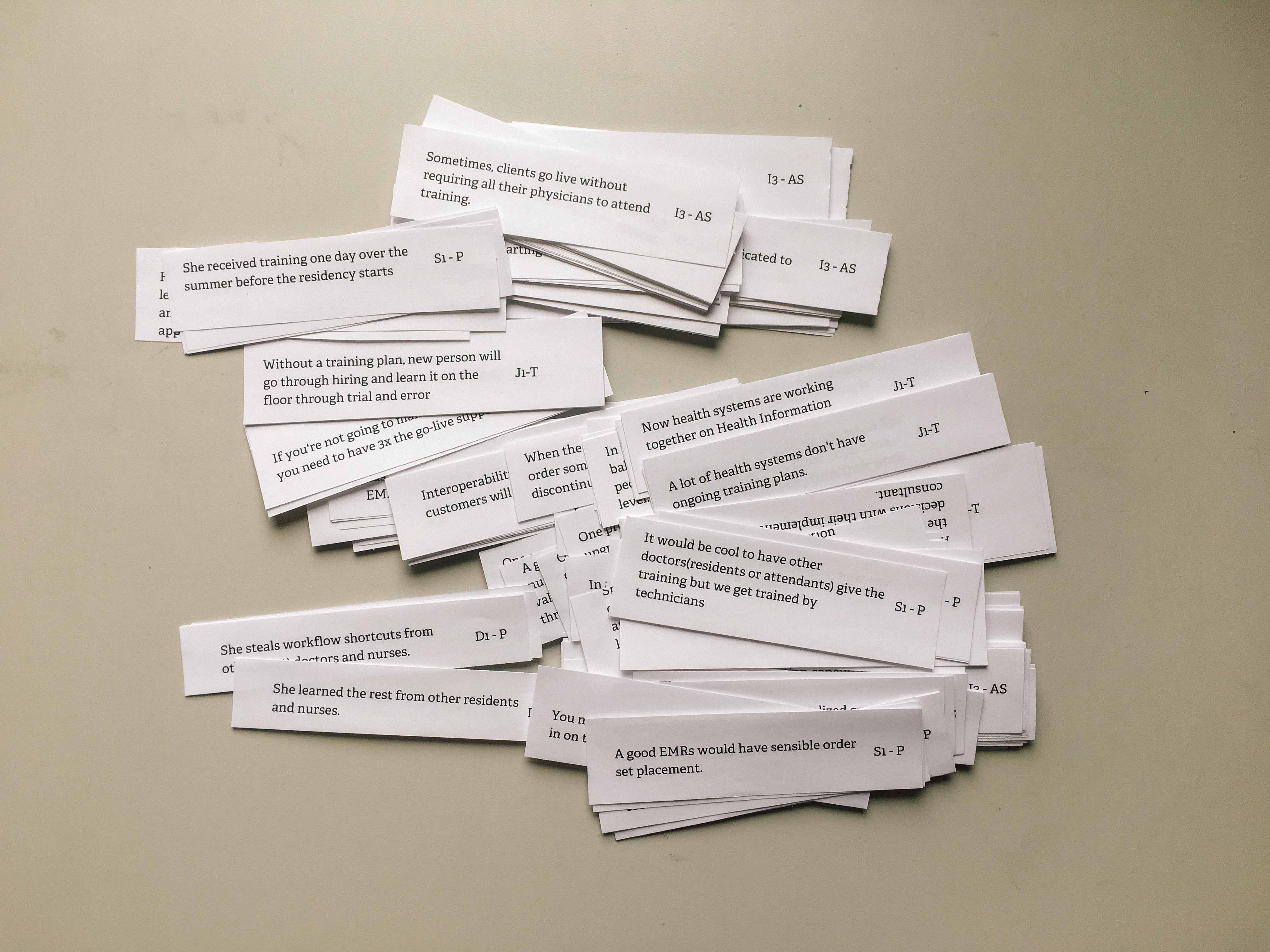
Surveying the Problem Landscape
Our first interviews showed us how little we knew about healthcare technology, and the financial and regulatory pressures surrounding healthcare organizations. We mapped out every unique entity in the healthcare industry that leverages or impacts electronic medical technology in the course of their work. Throughout the course of user interviews, we extracted bite-sized insights and codeified them in an affinity diagram. From here, we were able to pull out industry trends and takeaways that served as the basis for our design concepts down the road.
Accountable Care
The government is a unique stakeholder in this industry. In their efforts to manage the largest industry in the United States, they have passed multiple laws dictating what must be done when developing electronic medical records and incorporating it into clinical practice. Hospitals are incentivized to move from paper charts to software systems through laws such as MACRA and HITECH. On the other side of this service, EMR vendors themselves are under regulatory pressure to improve the usability of their product, as well as ensure that insurance companies (including the government) can receive structured documentation.
Industry Trends
Through interviews and hearing from industry leaders at HIMSS, we identified multiple high-level trends we feel EMR vendors will be impacted by over the next 5–10 years.
Consolidation
The notion of “accountable care organizations”, established in the Affordable Care Act, is a program that incentivizes different organizations in the healthcare industry—hospitals, private practices, insurers—to create strategic networks and optimize the delivery of patient care information. This has led to large medical systems purchasing private practices and driving up the cost of care—making it hard for smaller practices to pay for expensive EMRs and keep costs reasonable.
Interoperability
It is currently incredibly difficult to integrate personal health information between different medical systems—especially those on different EMRs. However, there are federal incentives for IT companies to improve this capability.
Analytics
Healthcare organizations want increased visibility into how their practice is performing, both from a revenue and patient outcomes perspective. At HIMSS, EMR vendors across the board touted their analytics dashboard solutions as a key selling point for health systems, and we quickly realized that data-driven and potentially artificially intelligent healthcare solutions will be competitive differentiators in the coming years.
Identifying Opportunity Areas
The conversation with Allscripts and the research helped us to identify the five key challenges we wanted to tackle in the implementation process:
- How do you help customers lead change?
- How do you reduce unnecessary customization?
- How do you scale training of providers?
- How do you improve overall product despite variation across instances?
- How do you use data to drive product decisions or workflow optimizations?
Each question led us to identify opportunity areas that can help improve client satisfaction and better patient outcome:
- Governance
- Workflow Design
- Provider Training
- Troubleshooting
- Continuous Improvement
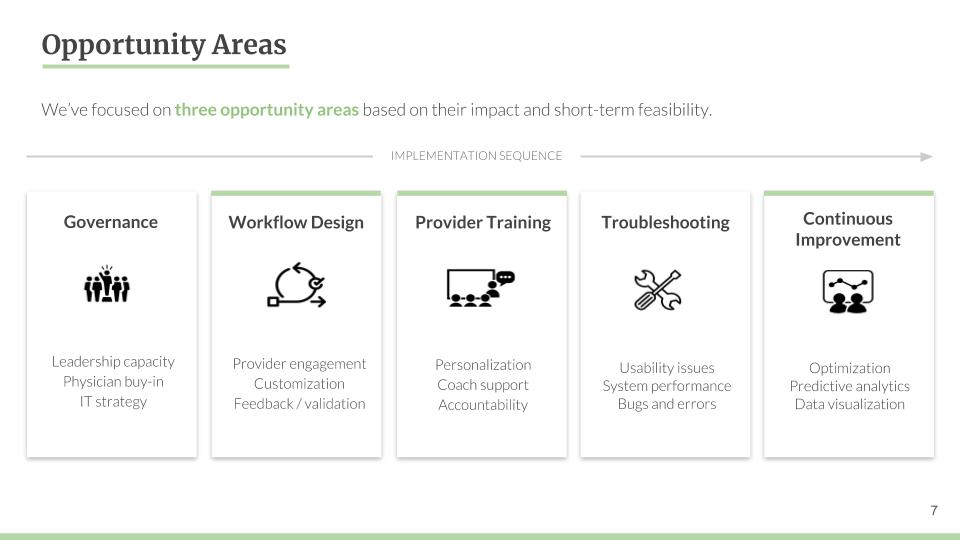
Out of the five opportunity areas, we initially focused on workflow design, provider training and continuous improvement considering the impact and short-term feasibility. Governance of Allscripts and the usability of Sunrise products are more long-term problems that were out of scope of our focus.
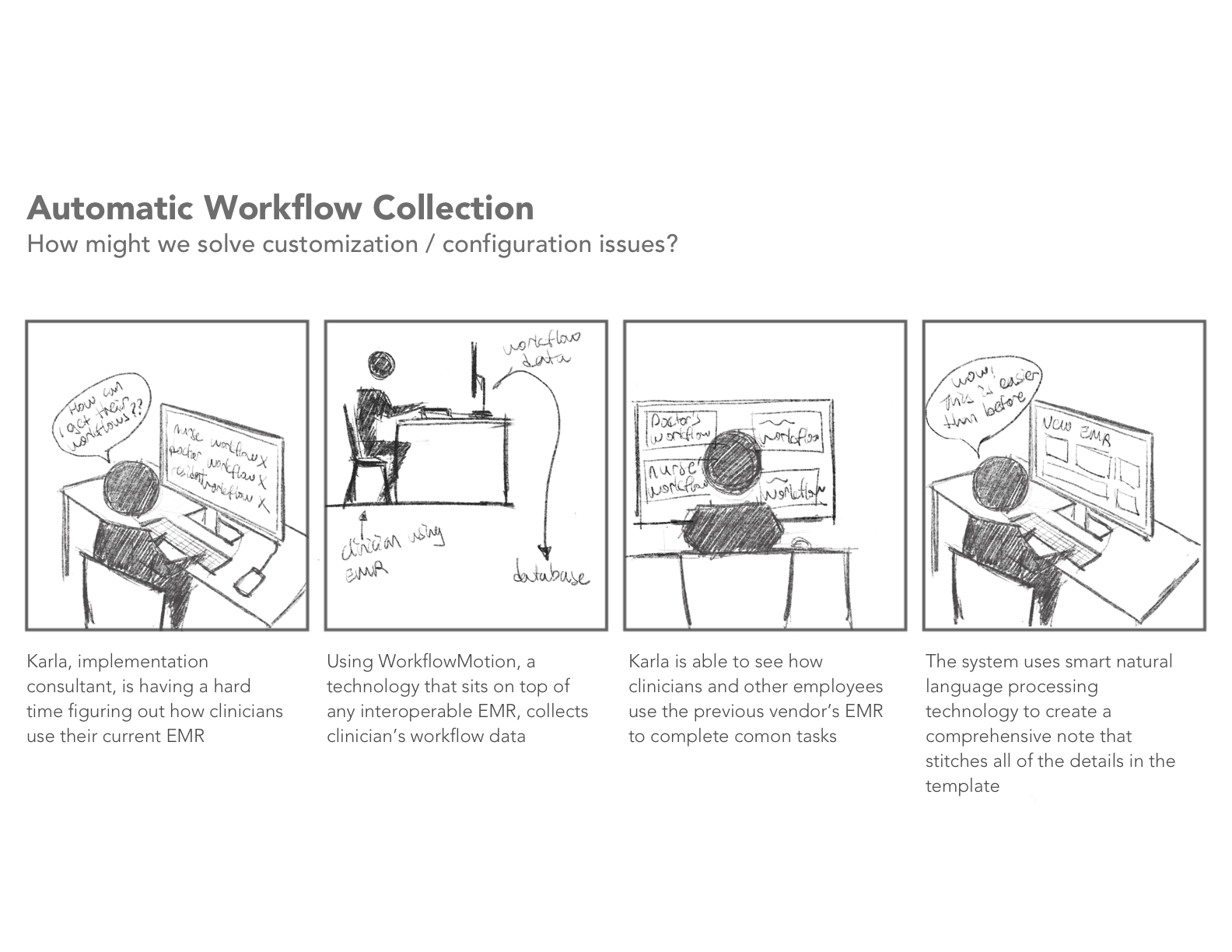
Workflow Design focuses on converging on EHR configuration design decisions to increase provider efficiency. The insights we have are:
- Providers don't want to engage in the EHR implementation process.
- Providers have strong opinions, which lead to overcustomization. This results in costly rework after the process is over.
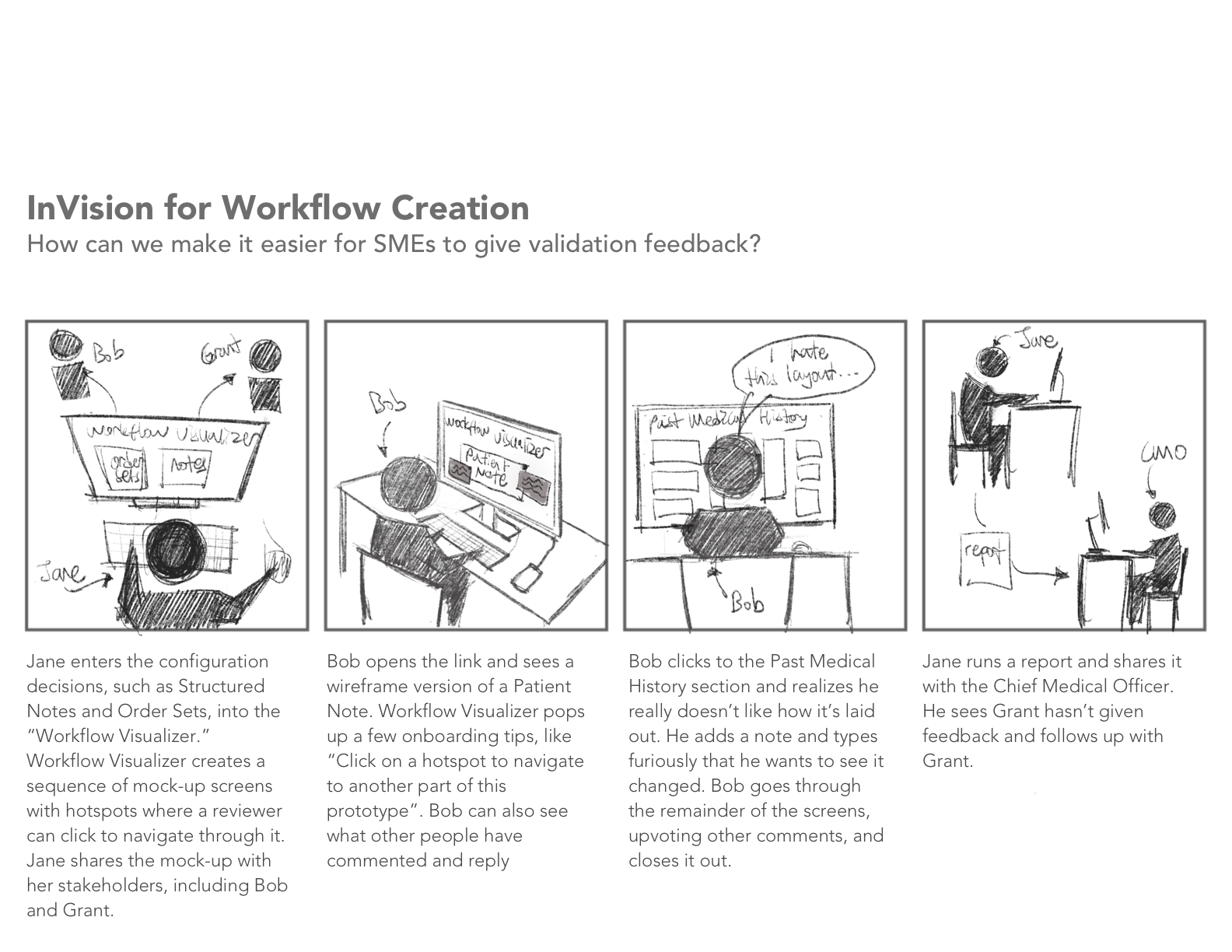
- The implementation consultant has to communicate with multiple differen stakeholders, and it's hard to get everyone to
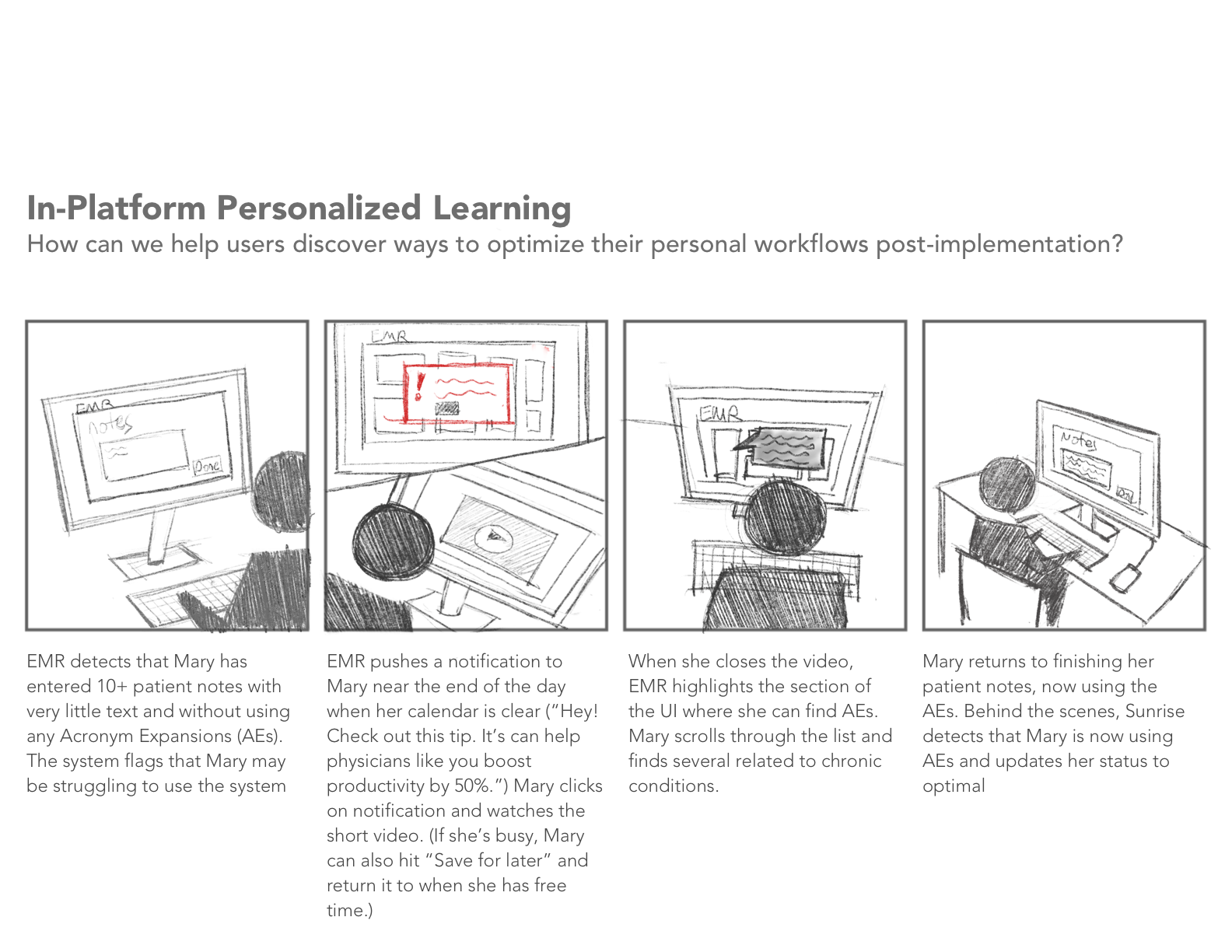
Provider Training focuses on delivering effective learning that is personalized to the individual needs of providers. The insights we have are:
- Providers often don’t have a formal ongoing training program, relying on ad hoc help requests.
- Providers want training for their specific workflow, but this is challenging due to Sunrise customizations.
- Providers like peer learning, but this tends to be reactive and self-selective. It can also overburden busy colleagues.
Continuous Improvement focuses on optimizing workflows to improve patient outcomes and physician satisfaction. The insights we have are:
- Workflow optimization is critical, but requires infrastructure, processes, and expertise.
- Struggling organizations change workflows based on ad hoc requests from providers.
- Workflow optimization using predictive analytics is increasingly a competitive differentiator.
Decisions and Takeaways
We decided to focus on workflow design, out of the three opportunity areas, primarily because improving workflow design can solve upstream problems such as training and physician burnout, affecting client satisfaction and patient outcomes.
A lack of transparency on workflow design leads to weak training. When workflow validation is left to the last minute, training gets short changed and pushed to the side, becoming a quick afterthought. In order to improve training, workflow design has to be solved.
Imprecise, inefficient workflows result in physician burnout. When a workflow doesn’t reflect a physician’s mental model and real-time documentation process, it often results in physicians lingering around work for an hour or two to finish documentation. It often looks something like this.