Working alongside University Hospitals in Cleveland, our group of Masters in Human-Computer Interaction students worked for four months to navigate secondary, primary, exploratory, generative, and evaluative research to redefine our problem space and offer valuable insights.
01
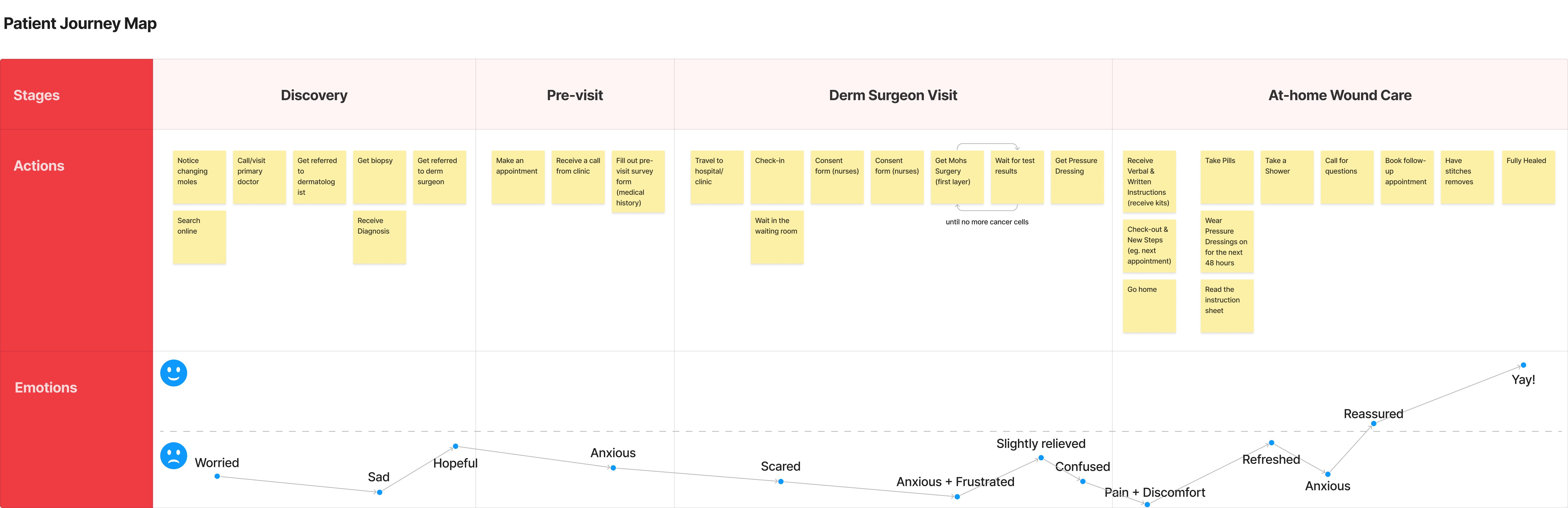
Before we dive into the gist of what we did and what we learned, we wish to take you on a ride to the journey of a typical patient with a surgical wound from a Mohs surgery.
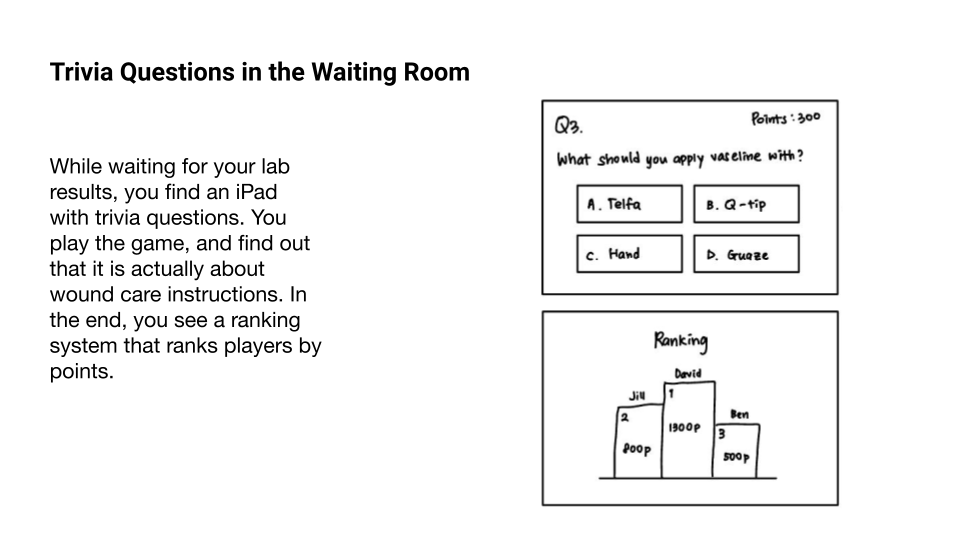
Mohs surgery↗ is essentially a procedure that involves removing the cancer tissues layer by layer. After being removed, each layer is sent to an on-site lab to determine if further layers need to be removed. While waiting for the result of each layer, patients typically need to wait for about 30 minutes to an hour.
Below is an initial patient journey map that we created to understand the patient's experience and emotions from the discovery stage to healing, and opportunities that may be found along the way.
02
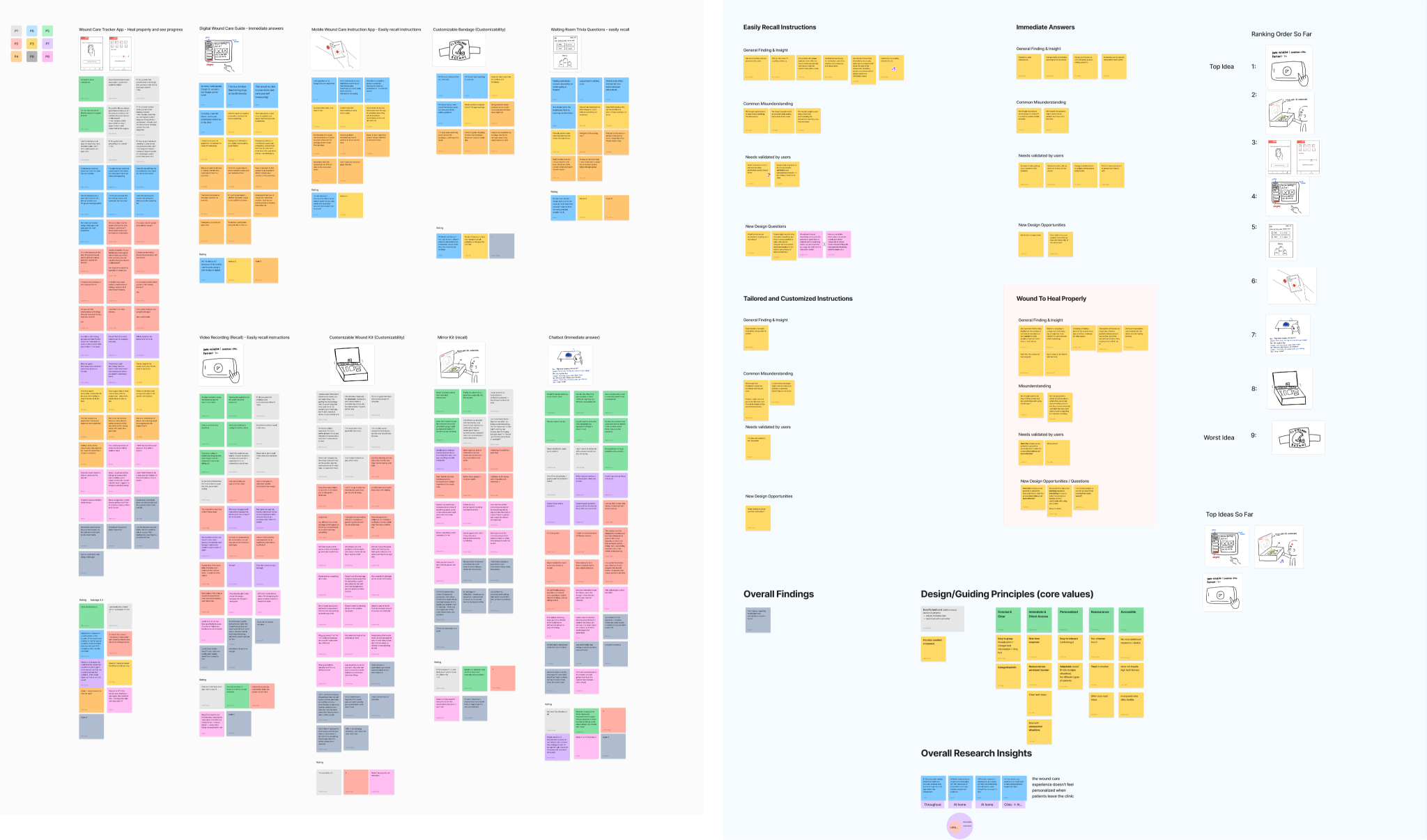
As we continued to analyze and synthesize the data we had collected over the course of the semester it became clear that we were faced with a different problem than we had originally set out to solve: the patient’s inability to deal with unexpected situations, and the lack of easily accessible, personalized information, are the main causes of poor surgical outcomes and healthcare providers’ burden.
the patient’s inability to deal with unexpected situations
the lack of easily accessible, personalized information
We understand our problem, and we know what the benefits will look like for our different stakeholders, so what questions do we have to guide our research as we move into the summer semester? Our team developed 2 ‘how might we’ questions that we believe, at this stage of our research, address the essence of our project:

How might we help patients to put more trust and attention towards the wound-care material?


How might we ensure patients receive immediate answers and reassurance while reducing the workload for nurses?

We didn’t just pull these guiding questions out of thin air, so to better understand how we got here we will get into our three key insights.
03
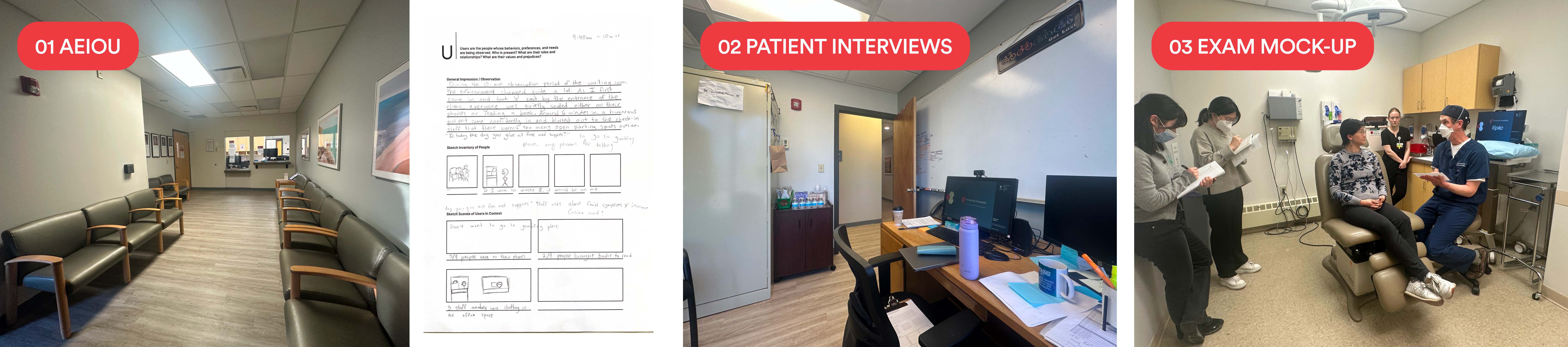
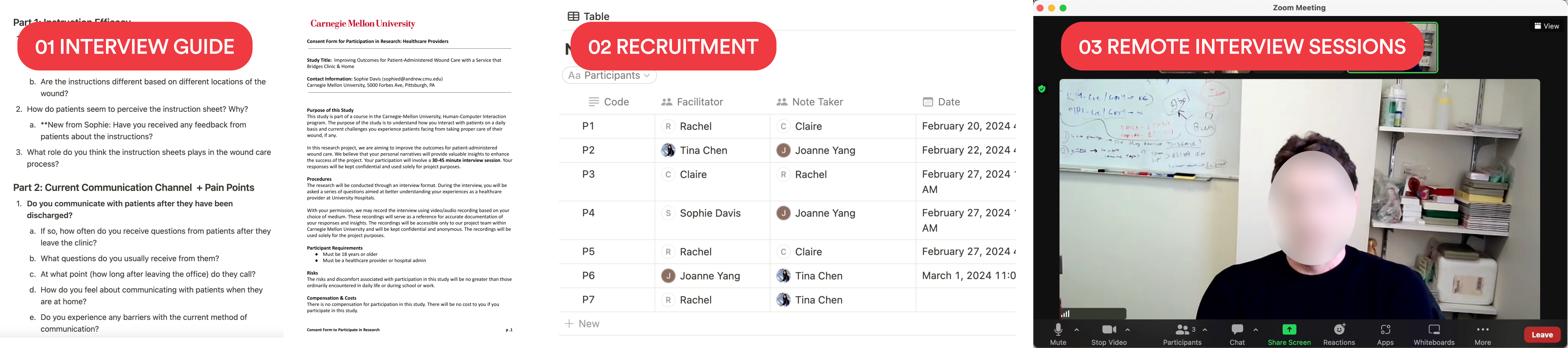
To answer these questions, we conducted a comprehensive research series that help us step into the world of wound care. Most excitingly, we began with a one-week empathy study to put ourselves in patients' shoes and become familiar with general wound care procedures. We also conducted site visits where we interacted with patients and healthcare providers in clinical settings to identify various touch points in this journey. Additionally, we interviewed both healthcare providers and patients to uncover pain points from both perspectives, and with speed dating sessions we showcased our ideas to explore hidden needs and potential design directions worth pursuing.
1-week
Empathy Study
6
Patient Interviews
& Site Visit
9
Expert Interviews
9
Speed Dating
& Interviews
04
01

The current wound care procedure doesn’t feel personalized beyond the clinic.
INTERVIEW
Nurses disclosed that they primarily use the wound care instruction sheet as a reference point, often tailoring the delivery of wound-care instructions based on various patient factors, including age, personality, cognitive ability, wound location, and prior experiences with wound care. They adjust aspects such as pacing, content coverage, and repetition frequency accordingly.
SITE VISIT
Concurrently, patients reported modifying their wound-care routines at home, such as trimming bandages or wearing long sleeves to bed. However, patients are not informed about these potential adjustments or provided guidance on how to personalize their care accordingly. Instead, they receive standardized wound care instructions that offer a general step-by-step guide. Consequently, patients are left to customize their experiences based on their own intuition and assumptions.
LITERATURE
REVIEW
Research highlights the significance of personalized care tailored to individual patient needs in maximizing satisfaction and treatment outcomes. For instance, patients who received customized printed and mobile-accessible emergency department (ED) discharge instructions for pain relief reported enhanced recall of pain relief medication advice.
To truly enhance wound care outcomes, it is important to extend personalization beyond the clinic setting by anticipating patients' needs during the immediate post-discharge period. For example, anticipating patients' cognitive ability entails recognizing that some individuals may require simplified instructions or additional support to comprehend and adhere to their wound care regimen effectively. Additionally, considering variations in patients' health and technology literacy levels, as well as their learning preferences, healthcare providers may offer materials in diverse mediums and modalities.
By proactively addressing these factors, patients will be more confident navigating their post-discharge care, ultimately improving outcomes and satisfaction with the wound care experience.
02

Although patients show high confidence for at-home wound care, they are unprepared when unexpected situations arise.
SITE VISIT
When asked about the level of confidence in their ability to perform wound care at home, 100% of the patients gave themselves a perfect score of 5 out of 5.
INTERVIEW
Nurses emphasized the importance of instilling confidence in patients before they leave the clinic. As Nurse 2 emphasized, “The goal is to make them (patients) feel confident about understanding the wound care procedure before they leave the clinic.” To achieve this, some nurses would streamline the information provided, focusing only on the essential steps of wound care while disregarding the rest about handling complications. For example, Nurse 4 mentioned that “I personally will only go over the first page. Most the information is on it, including what to do within the first week after surgery.”
OBSERVATION
However, as we delved into the call log data, we discovered that a significant 42% of the calls were related to complications, ranging from concerns about wound reopening to symptoms like itching and the appearance of white spots.
Therefore, other than continually making patients feel in control, we also want them to acknowledge that uncertainty is a natural part of the wound healing process, and more mindful of the potential complications that might arise as well as the corresponding ways to deal with them. By preparing patients to expect and handle potential complications, we aim to reduce anxiety and empower them with problem-solving skills to navigate challenges effectively throughout their recovery journey.
03

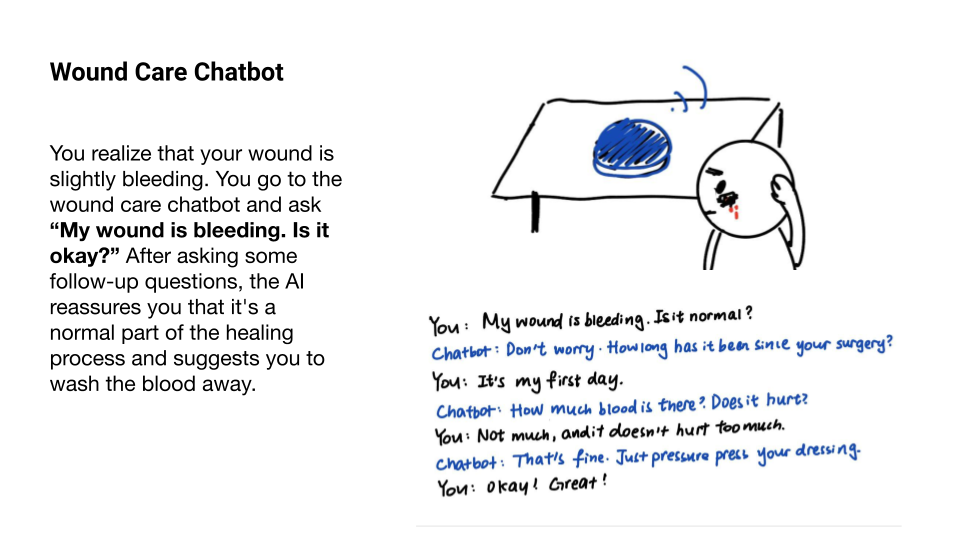
Patients seek constant reassurance from direct conversations with trusted healthcare providers.
INTERVIEW
In our interviews with experts, N out of 9 interviewees emphasized the importance of reassurance in their interactions with patients. In an interview, Nurse 2 emphasized that “it’s important to reassure them because people might easily forget or feel nervous.” Similarly, Nurse 5 quoted that “I always encourage patients, especially those living alone with challenging wound locations, to call me for feedback, reassurance, or further counseling.”
SPEED
DATING
According to Fareed's literature, patients often find reassurance when they feel nurses are simply 'there' for them, whether physically or easily accessible. At the Cleveland Clinic, phone call was the most common way patients sought reassurance. In speed dating sessions, 14 out of 16 patients stated they would first call nurses and doctors if they encountered any problems. Meanwhile, when asked about leveraging emerging technology like chatbots or mobile apps, many patients expressed discomfort and a lack of trust, indicating a preference for direct interaction.
SPEED
DATING
We discovered that patients heavily rely on calls due to their immense trust in healthcare providers' expertise and understanding of their situations. Patient 1 emphasized this trust, saying, “Usually, what they say can happen is what happens. If they tell me I can shower, I shower. Just like they told me.” Patient 8 echoed this sentiment, stating, “The doctor knows me, so I'd trust him. Right now, he is the expert.”
Therefore, other than continually making patients feel in control, we also want them to acknowledge that uncertainty is a natural part of the wound healing process, and more mindful of the potential complications that might arise as well as the corresponding ways to deal with them. By preparing patients to expect and handle potential complications, we aim to reduce anxiety and empower them with problem-solving skills to navigate challenges effectively throughout their recovery journey.