CHI 2016 Preview: HCII Researchers Get to the Heart of the Matter
If there's anywhere machine intelligence would seem to fit perfectly, it's healthcare. The rise of electronic medical records combined with advancements in big data technologies creates a field ripe for algorithm-powered tools that help clinicians make important decisions. But while these decision support tools (DST) are great in theory, they frequently fail in practice. Health researchers believe this failure stems from a lack of attention to human-computer interaction techniques, like understanding clinical workflow and the role AI plays in clinical practice.
A team of CMU researchers hopes to reverse that trend through efforts to help design a DST that supports clinicians working with heart patients who may need a ventricular assist device (VAD). In their paper, "Investigating the Heart Pump Implant Decision Process: Opportunities for Decision Support Tools To Help," the team outlines the details of a field study they performed to understand the clinical decision-making process and identify key touch points where clinicians may find a DST useful. The work, which received an honorable mention award, will be presented at the upcoming Association for Computing Machinery Conference on Human Factors in Computing Systems (CHI 2016), May 7–12 in San Jose, Calif. Authors include HCII Ph.D. student Qian Yang, HCII Associate Professor John Zimmerman, Associate Research Professor of Robotics Aaron Steinfeld, Biomedical Engineering Research Associate Lisa Carey and Biomedical Engineering Professor James Antaki.
Working with three different hospitals, the researchers interviewed and observed clinicians caring for patients in various stages of heart failure who were awaiting VAD implants. Their findings showed that, for most patient cases, VAD physicians don't consider the decision of whether to implant a VAD challenging and don't see a need to engage with a DST for help. "Clinicians are unlikely to use a tool that only does the easiest part of their job: telling them a textbook case is textbook,'" the authors wrote.
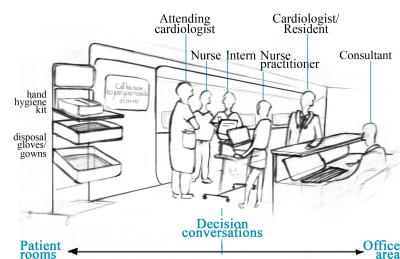
Most DSTs are programmed to take data and make a quantitative decision based on it. But VAD cases offer more ambiguity and rely on social evidence that goes beyond the data in the patient's electronic medical record. Instead, clinicians are more likely to consult colleagues for advice and second opinions, and are disinclined to trust computation in clinical settings. The teamwork involved in patient care and the safety regulations in hospitals (think: hand-washing) also make accessing a computer difficult at decision-making time.
With such facts stacked against DSTs, their future in clinical healthcare settings seems bleak. But the CMU field study discovered that such technology could be adapted to provide useful, meaningful feedback in a clinic. In a VAD clinic, a DST can respond to the culture by integrating automatically with the electronic medical record and streamlining patient information for weekly team decision-making meetings.
DSTs can also help provide more integrated support for VAD patients. Patients take different trajectories, with some arriving at implant facilities after years of careful monitoring, and some coming from emergency rooms. A DST could help coordinate patient data across doctors, and an intelligent system could monitor patients to ensure they adhere to lifestyle recommendations and receive help before it's too late to receive an implant.
Finally, the team concluded that DSTs need to combine machine intelligence with that of the human experts attending the patients. "Many of our participants implied that makers of current prognostic systems want to replace their expertise with inhuman technology," the researchers wrote. "Clearly there are opportunities for designing new interactions between DSTs and clinicians that work to integrate the abilities of both agents." Some of their ideas include collecting patient data across implant centers to better treat emergency cases, and connecting general cardiology physicians to implant centers to generate new referral relationships.
Mostly, though, HCI researchers need to fill the obvious gap between DSTs and clinical practice.
"DST development teams should work closely with HCI researchers and practitioners in search of near-term, pragmatic solutions to breach acceptance barriers," the team writes. "There is also a real need for HCI researchers to investigate clinical decision-making in various healthcare settings to enable the design of real-world-ready DSTs.
Read the full paper on ResearchGate. Learn more about the HCII at CHI 2016.
Story by Susie Cribbs (DC 2000, 2006)

